Premature ventricular contractions (PVCs) represent one of the most common cardiac arrhythmias encountered in clinical practice, affecting millions of individuals worldwide. These irregular heartbeats originate from the ventricles rather than the natural pacemaker, creating that distinctive “skipped beat” sensation many patients describe. While traditionally viewed through a purely cardiac lens, emerging evidence suggests a fascinating connection between gastrointestinal disorders and ventricular ectopy. The relationship between gastroesophageal reflux disease (GERD) and PVCs has garnered increasing attention from both cardiologists and gastroenterologists, revealing complex physiological pathways that interlink digestive and cardiac function in ways previously underappreciated.
Patient testimonials frequently describe a temporal relationship between acid reflux episodes and increased PVC frequency, with many reporting that gastrointestinal symptoms often precede or accompany their cardiac irregularities. This observation has prompted researchers to investigate the underlying mechanisms that might explain how stomach acid and oesophageal inflammation could potentially influence cardiac rhythm stability. Understanding these connections holds significant implications for treatment approaches and patient management strategies.
Understanding premature ventricular contractions and gastroesophageal reflux disease pathophysiology
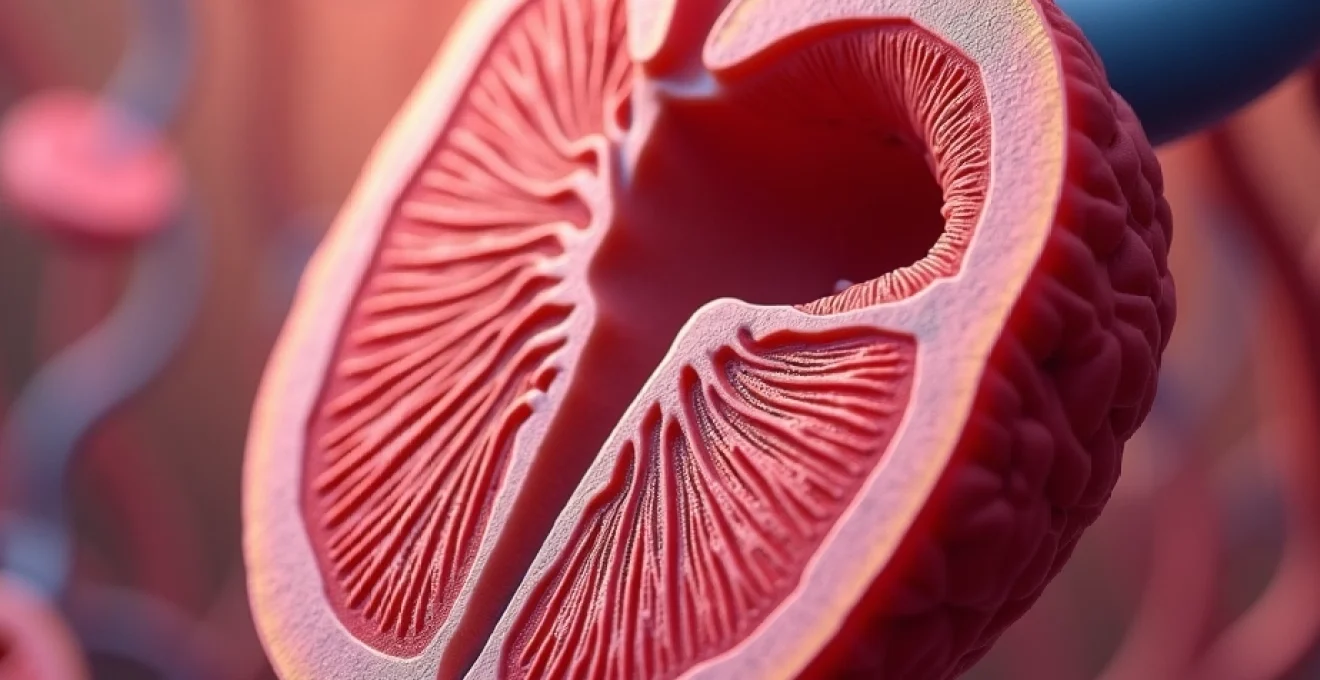
The pathophysiology underlying both PVCs and GERD involves complex interactions between multiple organ systems, creating potential crossover points where one condition might influence the other. Premature ventricular contractions occur when abnormal electrical impulses originate from the ventricular myocardium, disrupting the heart’s normal rhythm. These ectopic beats can manifest as isolated events or present in patterns such as bigeminy, trigeminy, or more complex arrangements that patients often describe as particularly unsettling.
Electrophysiological mechanisms of PVC generation in ventricular myocardium
The generation of PVCs involves disruption of normal cardiac conduction pathways, typically arising from enhanced automaticity, triggered activity, or re-entry mechanisms within ventricular tissue. Enhanced automaticity occurs when ventricular cells develop spontaneous depolarisation capabilities, effectively competing with the sinoatrial node’s natural pacemaking function. This phenomenon can be exacerbated by various factors including electrolyte imbalances, sympathetic nervous system activation, or inflammatory mediators circulating within the cardiovascular system. The sodium-potassium pump dysfunction often underlies these electrical disturbances, creating an environment conducive to ectopic beat formation.
Gerd-induced oesophageal inflammation and vagal nerve stimulation pathways
Gastroesophageal reflux disease creates a cascade of inflammatory responses within the oesophageal mucosa, involving prostaglandin release, cytokine activation, and direct tissue irritation from gastric acid exposure. The oesophagus shares intimate anatomical relationships with cardiac structures, particularly through vagal innervation patterns that can transmit inflammatory signals from the digestive tract to cardiac tissues. Vagal nerve stimulation resulting from oesophageal irritation may trigger reflexive changes in heart rate variability and potentially predispose individuals to ventricular arrhythmias through altered autonomic nervous system balance.
Histamine H2 receptor activation and cardiac rhythm disturbances
The histamine pathway plays a crucial role in both gastric acid production and cardiac function, with H2 receptors present throughout the cardiovascular system. When GERD triggers excessive histamine release, these mediators can directly influence cardiac conduction pathways, potentially affecting the stability of ventricular electrical activity. Research indicates that histamine can alter calcium channel function within cardiac myocytes, creating conditions that favour the development of triggered activity and subsequent PVC formation.
Acetylcholine release and parasympathetic modulation of heart rate variability
The parasympathetic nervous system’s response to oesophageal irritation involves increased acetylcholine release, which can significantly impact cardiac rhythm stability. This neurotransmitter affects both atrial and ventricular tissues, though its influence on ventricular ectopy remains complex and multifaceted. Acetylcholine-mediated effects on heart rate variability can create windows of vulnerability where PVCs are more likely to occur, particularly when combined with other predisposing factors such as electrolyte disturbances or concurrent medications.
Vagus Nerve-Mediated cardiac arrhythmia mechanisms in acid reflux patients
The vagus nerve represents the primary communication highway between the digestive system and the heart, carrying both afferent and efferent signals that can profoundly influence cardiac rhythm. In patients with chronic acid reflux, persistent vagal stimulation creates a state of heightened autonomic reactivity that may predispose individuals to various cardiac arrhythmias, including PVCs. This connection helps explain why many patients report increased ectopic beats during or shortly after meals, particularly those involving acidic or spicy foods that exacerbate reflux symptoms.
Oesophago-cardiac reflex arc and afferent vagal stimulation
The oesophago-cardiac reflex represents a well-documented physiological phenomenon where oesophageal stimulation triggers reflexive cardiac responses through vagal pathways. When stomach acid irritates the oesophageal mucosa, mechanoreceptors and chemoreceptors within the tissue generate afferent signals that travel via the vagus nerve to the cardiac control centres in the brainstem. These signals can subsequently trigger efferent responses that alter heart rate, contractility, and electrical conduction patterns, potentially creating the substrate for PVC development.
Neurotransmitter cascade effects on sinoatrial node function
The neurotransmitter cascade initiated by oesophageal irritation extends beyond simple vagal stimulation to involve complex interactions between multiple signalling molecules. Neuropeptides released during this process can influence sinoatrial node function, altering the heart’s natural pacemaking activity and creating opportunities for ectopic foci to emerge. Substance P, vasoactive intestinal peptide, and other neuropeptides released during GERD episodes may contribute to the electrical instability that facilitates PVC formation.
Inflammatory cytokine release and cardiac conduction system impact
Chronic oesophageal inflammation associated with GERD triggers the release of various inflammatory cytokines, including tumour necrosis factor-alpha, interleukin-6, and C-reactive protein. These inflammatory mediators can circulate systemically and potentially affect cardiac conduction system function, creating an environment that favours the development of ventricular arrhythmias. The inflammatory state may also alter calcium handling within cardiac myocytes, contributing to the triggered activity that underlies many PVCs.
Gastro-oesophageal junction distension and mechanoreceptor activation
The gastro-oesophageal junction contains numerous mechanoreceptors that respond to pressure changes and distension associated with reflux episodes. When gastric contents reflux into the oesophagus, these mechanoreceptors trigger vagal reflexes that can influence cardiac function. Mechanoreceptor activation may be particularly relevant in patients with hiatal hernias, where anatomical distortion creates persistent stimulation of these sensory pathways, potentially contributing to chronic PVC susceptibility.
Clinical evidence linking gastroesophageal reflux disease to ventricular ectopy
Clinical studies have provided compelling evidence supporting the relationship between GERD and increased PVC frequency, though the mechanisms remain incompletely understood. Observational studies consistently demonstrate higher rates of ventricular ectopy in patients with documented gastroesophageal reflux disease compared to control populations. One particularly noteworthy study found that patients with severe GERD experienced a 40% higher incidence of PVCs during 24-hour monitoring periods compared to individuals without reflux symptoms. This correlation persisted even after controlling for other cardiovascular risk factors, suggesting an independent relationship between digestive and cardiac symptoms.
Patient case studies further illuminate this connection, with many individuals reporting distinct patterns of PVC occurrence that correlate with their meals and reflux episodes. Temporal clustering of ventricular ectopy around periods of active acid reflux has been documented in multiple case series, providing real-world evidence for the theoretical mechanisms discussed in laboratory studies. The phenomenon known as gastrocardiac syndrome, or Roemheld syndrome, represents the most severe manifestation of this gut-heart connection, where gastrointestinal disturbances can trigger significant cardiac arrhythmias requiring medical intervention.
Research indicates that treating GERD with proton pump inhibitors can reduce PVC frequency by up to 60% in some patients, suggesting a direct therapeutic relationship between acid suppression and cardiac rhythm stability.
The evidence becomes even more compelling when examining the response to GERD treatment. Multiple studies have documented significant reductions in PVC frequency following successful acid reflux management with proton pump inhibitors or surgical interventions. This therapeutic response provides perhaps the strongest clinical evidence for a causal relationship, as addressing the underlying gastroesophageal pathology leads to measurable improvements in cardiac symptoms. However, the response is not universal, indicating that individual patient factors and the severity of both conditions play important roles in determining treatment outcomes.
Diagnostic approaches for GERD-Associated cardiac arrhythmias
Diagnosing the relationship between GERD and PVCs requires a comprehensive approach that simultaneously evaluates both cardiovascular and gastrointestinal function. The challenge lies in establishing temporal relationships between reflux episodes and cardiac symptoms, necessitating sophisticated monitoring techniques that can capture both physiological processes over extended periods. Modern diagnostic approaches increasingly employ combined monitoring strategies that provide unprecedented insights into the gut-heart connection in individual patients.
24-hour holter monitor correlation with ph impedance studies
The gold standard for establishing GERD-PVC relationships involves concurrent 24-hour Holter monitoring and oesophageal pH impedance studies. This combined approach allows clinicians to directly correlate acid reflux episodes with cardiac rhythm disturbances, providing objective evidence for the temporal relationships that patients often describe subjectively. pH impedance technology can detect both acidic and non-acidic reflux events, while modern Holter monitors capture every heartbeat with precise timing information, enabling detailed analysis of the relationship between digestive and cardiac events.
Ambulatory electrocardiography during proton pump inhibitor therapy
Monitoring cardiac rhythm before, during, and after proton pump inhibitor therapy provides valuable diagnostic information about the GERD-PVC relationship. Patients who demonstrate significant reductions in ventricular ectopy following acid suppression therapy likely have a genuine connection between their digestive and cardiac symptoms. This diagnostic approach is particularly useful because it serves dual purposes: confirming the relationship while simultaneously providing therapeutic benefit for patients with confirmed GERD-associated arrhythmias.
Upper endoscopy findings and concurrent cardiac rhythm analysis
Upper endoscopy performed with concurrent cardiac monitoring can reveal important correlations between the severity of oesophageal inflammation and cardiac rhythm disturbances. Patients with severe oesophagitis often demonstrate higher baseline PVC frequencies and greater rhythm variability during endoscopic procedures. Endoscopic findings such as Barrett’s oesophagus, strictures, or severe mucosal inflammation may correlate with increased susceptibility to GERD-associated cardiac symptoms, helping clinicians stratify patients who might benefit most from aggressive reflux management.
Pharmacological interventions and PVC frequency reduction strategies
Treatment approaches for GERD-associated PVCs typically involve addressing the underlying gastroesophageal pathology while simultaneously managing cardiac symptoms when necessary. Proton pump inhibitors represent the first-line therapeutic intervention, with studies demonstrating significant PVC reduction in 60-80% of patients who achieve adequate acid suppression. The mechanism likely involves reducing oesophageal inflammation and vagal irritation, thereby decreasing the stimulus for cardiac rhythm disturbances. Acid suppression therapy must be optimised for each individual, as subtherapeutic dosing may fail to provide cardiac benefits even when gastrointestinal symptoms improve.
H2 receptor antagonists may offer additional benefits beyond their gastric acid suppression effects, as these medications can directly influence cardiac H2 receptors that may contribute to arrhythmia susceptibility. Some patients experience better PVC control with combination therapy involving both proton pump inhibitors and H2 antagonists, though this approach requires careful monitoring for potential drug interactions and side effects. The timing of medication administration also plays a crucial role, with many patients benefiting from pre-meal dosing that prevents rather than treats reflux episodes.
Beta-blockers may provide dual benefits for patients with GERD-associated PVCs by reducing both cardiac irritability and gastric acid production through their effects on the autonomic nervous system.
When PVC symptoms persist despite adequate acid suppression, traditional cardiac medications may be necessary. Beta-blockers offer particular advantages in this population because they address both cardiac symptoms and may indirectly benefit GERD by reducing gastric acid production through autonomic modulation. Metoprolol and atenolol have shown efficacy in reducing PVC frequency while potentially providing gastrointestinal benefits, making them attractive options for patients with both conditions. Calcium channel blockers require careful consideration, as some formulations may exacerbate reflux symptoms by reducing lower oesophageal sphincter pressure.
Magnesium supplementation deserves special attention in this population, as many patients with chronic GERD develop magnesium deficiency due to proton pump inhibitor use or dietary restrictions. Magnesium plays crucial roles in cardiac electrical stability, and deficiency can significantly increase PVC frequency and severity. Regular monitoring of serum magnesium levels and appropriate supplementation can provide substantial symptom relief for many patients with GERD-associated cardiac symptoms.
Lifestyle modifications for managing acid Reflux-Induced cardiac symptoms
Lifestyle interventions form the cornerstone of management for patients experiencing GERD-associated PVCs, offering the potential for significant symptom relief without the risks associated with long-term medication use. Dietary modifications represent perhaps the most impactful intervention, with many patients experiencing dramatic improvements in both digestive and cardiac symptoms through careful attention to meal composition, timing, and portion sizes. Trigger food elimination often provides the most immediate relief, with common culprits including citrus fruits, tomatoes, chocolate, caffeine, and spicy foods that can exacerbate both reflux and cardiac symptoms.
Meal timing and positioning strategies can significantly influence the severity of GERD-associated cardiac symptoms. Avoiding large meals within three hours of bedtime prevents nocturnal reflux episodes that often trigger PVCs during sleep periods. Elevating the head of the bed by 6-8 inches using blocks or wedges helps maintain gravitational assistance in preventing acid reflux, potentially reducing overnight cardiac symptoms that many patients find particularly distressing. Eating smaller, more frequent meals throughout the day prevents gastric distension that can trigger both reflux and cardiac symptoms through vagal stimulation pathways.
Weight management plays a crucial role in managing both GERD and associated cardiac symptoms, as excess abdominal weight increases intra-abdominal pressure and promotes reflux episodes. Even modest weight loss of 5-10% of body weight can provide significant symptom relief for many patients. The relationship between obesity and GERD-associated PVCs appears multifactorial, involving mechanical factors, inflammatory mediators, and sleep-disordered breathing that can all contribute to increased cardiac irritability.
Stress management techniques deserve particular attention in this patient population, as psychological stress can exacerbate both gastrointestinal and cardiac symptoms through autonomic nervous system activation. Mindfulness meditation, deep breathing exercises, and regular physical activity can help modulate the stress response and potentially reduce both reflux episodes and cardiac symptoms. Patients who incorporate stress reduction techniques often report improved symptom control and better overall quality of life, suggesting that psychological factors play important roles in the manifestation and management of GERD-associated cardiac symptoms.