Dental trauma can manifest in various forms, and one of the most concerning yet often overlooked presentations is the bruised tooth. When trauma affects dental structures, the resulting damage may not always be immediately apparent through conventional visual examination alone. Understanding the visual characteristics of traumatised teeth becomes crucial for timely diagnosis and appropriate treatment intervention. The appearance of a bruised tooth can range from subtle discolouration changes to dramatic shifts in tooth colour that signal significant pulpal compromise.
Recognising these visual indicators requires a comprehensive understanding of both the underlying pathophysiology and the progressive nature of dental trauma. The complexity of dental pulp response to injury creates a spectrum of appearances that can evolve over time, making accurate assessment challenging even for experienced practitioners. Early identification of these changes can mean the difference between successful conservative management and the need for more invasive endodontic treatment.
Clinical identification of dental pulp necrosis and bruised tooth symptoms
The clinical presentation of dental trauma extends far beyond simple visual changes, encompassing a complex array of symptoms that may develop immediately following injury or emerge gradually over weeks to months. Patients frequently report initial pain that may subside temporarily, only to return with increased intensity as pulpal inflammation progresses. This characteristic pain pattern often confuses both patients and practitioners, as the apparent improvement may mask underlying tissue damage.
Thermal sensitivity represents one of the earliest and most reliable indicators of pulpal compromise following dental trauma. Patients typically experience prolonged pain responses to cold stimuli, which may persist for several minutes after the stimulus is removed. This hyperalgesia results from inflammatory mediator release within the confined pulpal space, creating pressure that sensitises nociceptive nerve endings.
Percussion sensitivity often accompanies thermal symptoms, manifesting as sharp pain when the affected tooth contacts opposing teeth during normal function or when tapped gently with an instrument. This symptom indicates involvement of the periodontal ligament and surrounding supporting structures, suggesting that the trauma has affected tissues beyond the pulp itself.
The progression from initial trauma to clinically apparent symptoms can vary dramatically between patients, making careful monitoring essential for accurate diagnosis and treatment planning.
Characteristic discolouration patterns in traumatised teeth
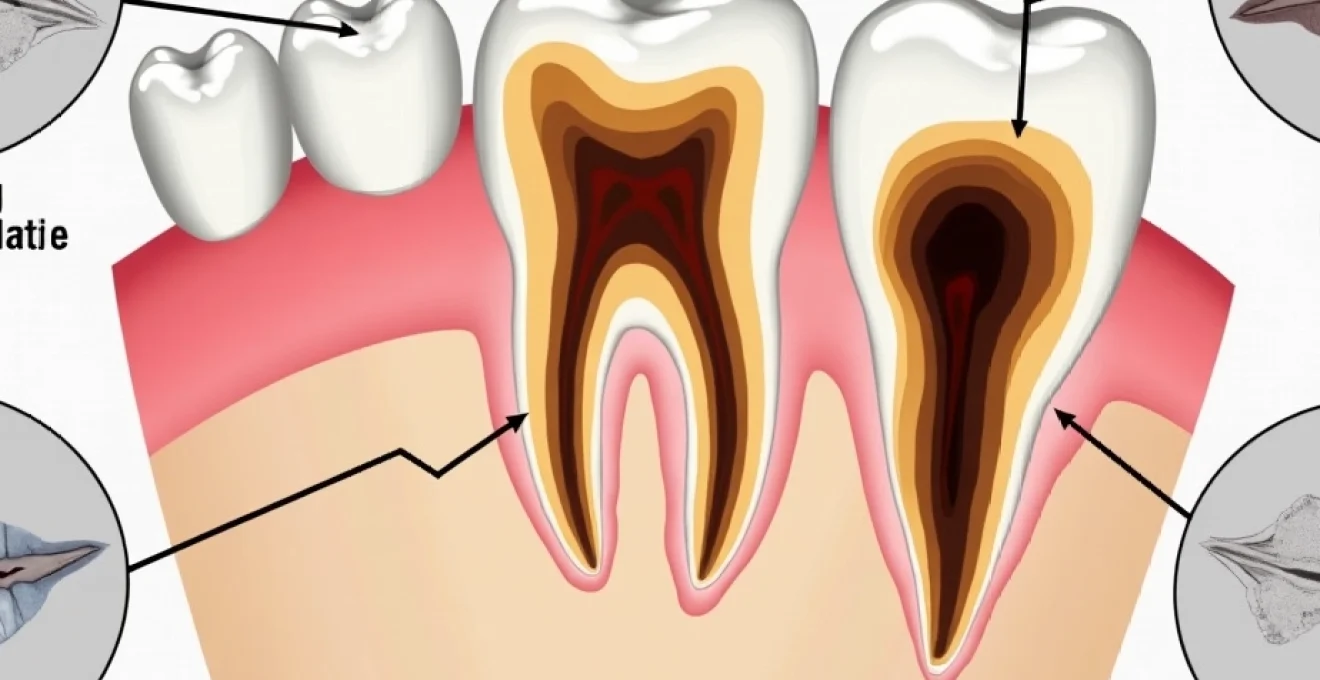
Dental discolouration following trauma follows predictable patterns that reflect the underlying pathological processes occurring within the pulpal tissues. The initial colour changes typically begin with subtle pink or purple hues that may be barely perceptible during routine clinical examination. These early changes result from capillary damage and haemorrhage within the pulpal chamber , creating the characteristic bruised appearance that gives this condition its common name.
The distribution of discolouration often provides valuable diagnostic information about the extent and severity of pulpal damage. Uniform discolouration throughout the clinical crown suggests widespread pulpal haemorrhage and potential necrosis, while localised colour changes may indicate more limited tissue damage with better potential for healing.
Grey-blue discolouration following pulpal haemorrhage
The development of grey-blue discolouration represents a critical milestone in the progression of dental trauma, typically indicating significant pulpal compromise with poor prognosis for spontaneous recovery. This distinctive colour change results from the breakdown of haemoglobin within the pulpal tissues, creating iron-containing compounds that impart the characteristic metallic appearance.
The timeline for grey-blue discolouration development varies considerably, with some teeth showing changes within days of trauma while others may not demonstrate visible alterations for several weeks. Progressive darkening over time generally correlates with advancing pulpal necrosis and the accumulation of breakdown products within the dentinal tubules.
Yellow-brown staining from haemoglobin breakdown products
Yellow-brown staining patterns often emerge as secondary changes following the initial grey-blue phase, representing continued decomposition of blood products within the pulpal space. These colour changes typically indicate advanced pulpal necrosis with significant tissue breakdown and the formation of various degradation products that penetrate the dentinal structure.
The intensity and distribution of yellow-brown staining can provide valuable prognostic information, with more extensive discolouration generally indicating poorer outcomes for conservative treatment approaches. Patients presenting with these colour changes typically require immediate endodontic intervention to prevent further complications.
Progressive darkening timeline in Non-Vital teeth
The chronological progression of tooth darkening follows a relatively predictable pattern, though individual variations can occur based on factors such as patient age, initial trauma severity, and pre-existing dental conditions. Understanding this timeline enables practitioners to make informed decisions about treatment timing and intervention strategies.
Initial discolouration typically becomes apparent within 2-4 weeks following trauma, beginning with subtle pink or purple hues that gradually intensify. The transition to grey-blue colouration usually occurs within 6-8 weeks, while yellow-brown staining may not develop until 3-6 months post-injury. Complete darkening to black or dark brown typically indicates end-stage pulpal necrosis with extensive tissue breakdown.
Radiographic evidence of dental trauma and pulpal damage
Radiographic examination provides essential complementary information that may not be apparent through clinical examination alone, particularly in cases where visual changes are subtle or have not yet developed. The radiographic appearance of traumatised teeth can reveal crucial details about pulpal health, root integrity, and surrounding bone structure that directly influence treatment decisions and prognosis.
Digital radiography has revolutionised the assessment of dental trauma by providing enhanced image quality and the ability to manipulate contrast and brightness to reveal subtle changes. These technological advances enable practitioners to detect early signs of pulpal compromise that might otherwise go unnoticed until more advanced symptoms develop.
The interpretation of radiographic findings requires careful consideration of baseline anatomy and an understanding of how trauma-related changes manifest on different imaging modalities. Systematic evaluation of pulpal space dimensions, root canal morphology, and periapical tissues provides a comprehensive picture of the extent of damage and guides appropriate treatment planning.
Periapical radiographic changes in bruised teeth
Periapical radiographic changes often represent the first detectable signs of pulpal compromise following dental trauma, appearing weeks or months before obvious clinical symptoms develop. These changes typically begin as subtle widening of the periodontal ligament space around the root apex, indicating inflammatory response within the surrounding tissues.
Progressive development of periapical radiolucency suggests advancing pulpal necrosis with bacterial invasion and the formation of chronic inflammatory lesions. The size and characteristics of these radiolucent areas provide valuable information about disease progression and the urgency of required intervention.
Cone beam CT imaging for root fracture detection
Three-dimensional imaging through cone beam computed tomography (CBCT) has become increasingly valuable for detecting root fractures and other structural damage that may not be visible on conventional radiographs. This advanced imaging modality provides detailed cross-sectional views of tooth structure and surrounding tissues, enabling precise localisation of fracture lines and assessment of their extent.
CBCT imaging proves particularly valuable in cases where clinical symptoms suggest significant trauma but conventional radiographs appear normal. High-resolution imaging can reveal hairline fractures, complex root anatomy, and three-dimensional relationships between damaged structures that influence treatment planning decisions.
Pulp canal obliteration on intraoral radiographs
Pulp canal obliteration represents a defensive response to trauma, characterised by progressive narrowing of the root canal space through continued dentine deposition. This radiographic finding appears as gradual reduction in pulpal space dimensions, often beginning at the apical third of the root and progressing coronally over time.
The rate of pulp canal obliteration varies considerably between patients and can provide valuable prognostic information about pulpal health. Rapid obliteration may indicate successful healing response, while slow or incomplete narrowing might suggest compromised pulpal vitality requiring intervention.
Lamina dura thickening and periapical lucency formation
Changes in the lamina dura, the radiopaque line surrounding the tooth root, often provide early radiographic evidence of trauma-related inflammation. Thickening of this structure indicates increased bone density resulting from chronic inflammatory stimulation and represents an important diagnostic finding in traumatised teeth.
The development of periapical lucencies represents more advanced pathological changes, typically indicating bacterial invasion of necrotic pulpal tissues and the formation of chronic inflammatory lesions. Careful monitoring of these changes helps determine the appropriate timing for endodontic intervention and guides treatment planning decisions.
Differential diagnosis between bruised teeth and alternative dental pathologies
Accurate diagnosis of bruised teeth requires careful differentiation from other dental pathologies that may present with similar clinical and radiographic findings. The overlap in symptoms between various conditions can create diagnostic challenges, particularly in the early stages when characteristic signs may not yet have fully developed. Understanding these differential diagnoses becomes crucial for appropriate treatment selection and patient management.
Carious lesions can sometimes mimic the symptoms of dental trauma, particularly when decay approaches the pulpal tissues and creates inflammatory responses. However, careful clinical examination typically reveals evidence of cavity formation or previous restorative work that helps distinguish between these conditions. Thermal testing patterns also differ, with carious teeth often showing immediate sharp pain responses rather than the prolonged aching associated with trauma.
Cracked tooth syndrome presents particular diagnostic challenges due to symptom similarities with bruised teeth, including percussion sensitivity and thermal responses. The key distinguishing features often lie in the pattern of pain provocation, with cracked teeth typically showing sharp pain on biting release rather than the constant aching associated with pulpal inflammation.
Periodontal disease can create symptoms that overlap with those of traumatised teeth, particularly regarding percussion sensitivity and radiographic changes around the root apex. Careful periodontal examination, including probing depths and mobility testing, helps differentiate between these conditions and identifies cases where both pathologies may coexist.
The complexity of dental pain and the potential for multiple concurrent pathologies requires systematic diagnostic approaches that consider all possible contributing factors.
Photographic documentation techniques for bruised tooth assessment
Comprehensive photographic documentation plays a vital role in monitoring the progression of tooth discolouration and communicating findings between practitioners and with patients. Standardised photography techniques ensure consistent documentation that enables accurate comparison over time and helps track treatment outcomes. The subtle nature of early colour changes in bruised teeth makes high-quality photography essential for detecting and monitoring these important clinical findings.
Digital photography equipment must be configured to provide accurate colour reproduction, typically requiring calibrated lighting systems and standardised camera settings. The use of colour correction cards and consistent positioning ensures that documented changes reflect actual clinical findings rather than variations in photographic technique. Standardised protocols for patient positioning, camera angles, and lighting conditions enable reliable comparison between successive appointments.
Close-up photography with appropriate magnification reveals subtle colour variations that may not be apparent during routine clinical examination. Macro lenses and ring flash systems provide the necessary detail and consistent illumination required for accurate documentation of early discolouration changes. The ability to enhance and manipulate digital images enables practitioners to highlight subtle findings that support diagnostic decisions.
Serial photography over time creates a valuable record of disease progression that guides treatment decisions and helps predict future developments. This documentation proves particularly valuable when determining the optimal timing for endodontic intervention or when monitoring conservative treatment approaches. Patient education also benefits significantly from visual documentation that clearly demonstrates the progression of pathological changes.
Emergency management protocols for suspected dental pulp trauma
Immediate management of suspected dental pulp trauma requires systematic assessment and prompt intervention to optimise outcomes and minimise long-term complications. The time-sensitive nature of pulpal injury makes rapid evaluation and appropriate initial treatment crucial for preserving tooth vitality and preventing the need for more extensive future procedures.
Initial assessment must include comprehensive trauma history, including mechanism of injury, timing, and any immediate symptoms experienced by the patient. Understanding the forces involved and the direction of impact provides valuable insight into the likely extent of damage and helps guide diagnostic priorities. Systematic examination protocols ensure that all relevant clinical findings are documented and appropriate baseline data established.
Pain management represents a critical component of emergency care, both for patient comfort and to enable thorough clinical examination. Appropriate analgesic protocols must balance effective pain relief with the need to preserve diagnostic sensitivity for clinical testing procedures. The selection of pain management strategies should consider both immediate relief and potential interactions with planned diagnostic procedures.
Provisional treatment measures may include occlusal adjustment to reduce traumatic contact, temporary splinting for mobile teeth, or placement of protective barriers over exposed dentinal surfaces. These interventions aim to minimise further damage while more comprehensive treatment plans are developed. Documentation of all emergency procedures and patient responses provides essential information for ongoing care coordination.
Long-term prognosis and monitoring requirements for traumatised teeth
The long-term prognosis for traumatised teeth depends on numerous factors, including the extent of initial damage, patient age, timing of intervention, and compliance with monitoring protocols. Understanding these prognostic factors enables practitioners to provide accurate patient counselling and develop appropriate long-term care plans that address both immediate needs and potential future complications.
Age-related factors significantly influence healing potential and treatment outcomes, with younger patients generally demonstrating better capacity for pulpal recovery following trauma. The continued root development in immature teeth provides additional treatment options and may enable conservative approaches that would not be suitable for mature teeth. Monitoring protocols must be adjusted based on patient age and developmental status to optimise outcomes.
Regular follow-up appointments enable early detection of complications and timely intervention when conservative management fails. The frequency and duration of monitoring depend on the severity of initial trauma and the chosen treatment approach, with more extensive injuries requiring longer observation periods. Standardised assessment protocols ensure consistent evaluation and enable reliable detection of progressive changes.
Patient education about long-term monitoring requirements proves essential for successful outcomes, as many complications develop months or years after initial trauma. Clear communication about warning signs that require immediate attention helps ensure appropriate utilisation of emergency dental services. The establishment of long-term relationships between patients and dental care providers facilitates effective monitoring and enables prompt intervention when complications arise.